Nota 99 AIFA
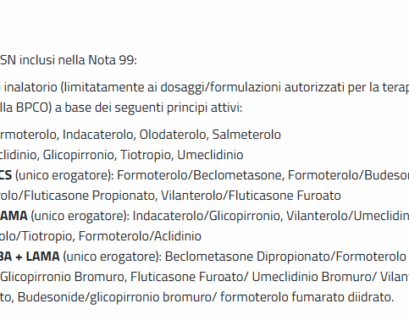
Note AIFAFarmaci in Nota: medicinali per uso inalatorio (limitatamente ai dosaggi/formulazioni autorizzati per la terapia inalatoria di...
Nota 1 AIFA
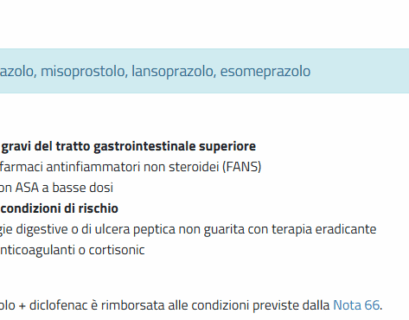
Note AIFAFarmaci in nota: pantoprazolo, omeprazolo, misoprostolo, lansoprazolo, esomeprazolo Riferimenti: https://www.aifa.gov.it/nota-01 La...
Nota 2 AIFA
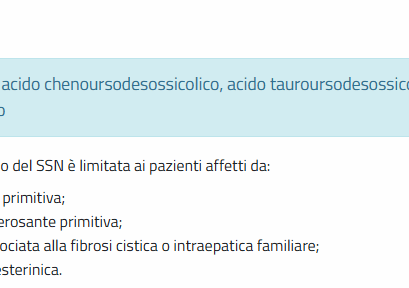
Note AIFAFarmaci in nota: acido chenoursodesossicolico, acido tauroursodesossicolico, acido ursodesossicolico Riferimenti:...
Nota 4 AIFA
Note AIFAFarmaci in nota: duloxetina, gabapentin, pregabalin Riferimenti: https://www.aifa.gov.it/nota-4 La prescrizione a carico del SSN è...
Nota 13 AIFA
Note AIFAFarmaci a carico SSN inclusi nella Nota 13: Ipolipemizzanti: Fibrati: bezafibrato, fenofibrato, gemfibrozil Statine: simvastatina,...
Nota 31 AIFA
Note AIFAFarmaco in nota: Levodropropizina, Diidrocodeina Acido benzoico, Diidrocodeina Riferimenti: https://www.aifa.gov.it/nota-31 La...
Nota 55 AIFA
Note AIFAFarmaci in nota: Tobramicina, Piperacillina + Tazobactam, Piperacillina, Netilmicina, Mezlocillina, Gentamicina, Ceftazidima, Cefepime,...
Nota 66 AIFA
Note AIFAFarmaci in nota: Tenoxicam, Sulindac, Proglumetacina, Piroxicam, Oxaprozina, Nimesulide, Naprossene, Nabumetone, Meloxicam, Lornoxicam,...
Nota 79 AIFA
Note AIFAFarmaci in nota: Teriparatide, Ranelato di stronzio, Raloxifene, Denosumab, Bazedoxifene, Acido risedronico, Acido ibandronico, Acido...
Nota 82 AIFA
Note AIFAFarmaci in nota: Zafirlukast, Montelukast Riferimenti: https://www.aifa.gov.it/nota-82 La prescrizione a carico del SSN è limitata alle...
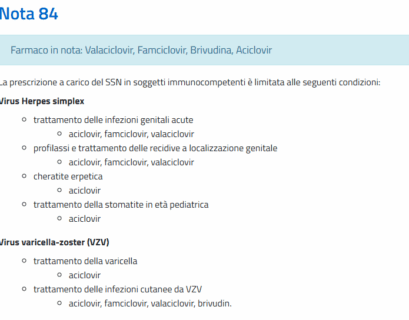
Nota 84 AIFA
Note AIFAFarmaci in nota: Valaciclovir, Famciclovir, Brivudina, Aciclovir Riferimenti: https://www.aifa.gov.it/nota-84 La prescrizione a carico...
Nota 87 AIFA
Note AIFAFarmaci in nota: Oxibutinina, Solifenacina, Tolterodina Riferimenti: https://www.aifa.gov.it/nota-87 Farmaci per l’incontinenza urinaria...
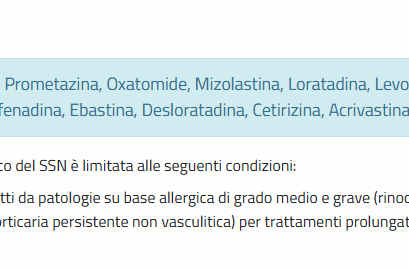
Nota 89 AIFA
Note AIFAFarmaci in nota: Prometazina, Oxatomide, Mizolastina, Loratadina, Levocetirizina, Ketotifene, Fexofenadina, Ebastina, Desloratadina,...
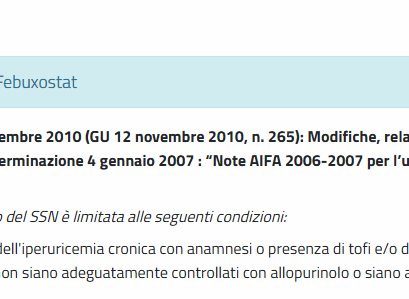
Nota 91 AIFA
Note AIFAFarmaci in nota: Febuxostat Riferimenti: https://www.aifa.gov.it/nota-91 Determinazione 2 novembre 2010 (GU 12 novembre 2010, n. 265):...