CMAJ: nuove linee guida sulla prevenzione dell’HIV prima e dopo l’esposizione
HIVSono ora disponibili trattamenti pre-esposizione multipla (PrEP) e post-esposizione (PEP) per prevenire l’infezione da HIV....
Aids, il «telefono verde» fa gli straordinari per contrastare fake news e stigma sul lavoro
In occasione della Giornata mondiale di Lotta contro l’Aids dell’1 dicembre il Telefono Verde Aids e Infezioni Sessualmente Trasmesse – 800861061, anonimo e gratuito – effettuerà un’apertura straordinaria dalle 9…
HIV in Italia: casi stabili, diagnosi tardive e prevenzione necessaria
Hiv – Alla vigilia della Giornata mondiale contro l’AIDS, in Italia i casi HIV restano stabili. Serve più prevenzione, test e accesso alla PrEP long acting.
Observations from ID and Beyond: ID Things to Be Grateful for — 2025 Edition
Dr. Paul Sax shares a half-dozen solid ID things we can be grateful for as we head into the holiday season, in HIV and ID Observations.
Epatite C: aggiornamento del 24 novembre 2025 sui pazienti arruolati
L’Agenzia Italiana del Farmaco rende disponibile l’aggiornamento settimanale dei dati relativi ai trattamenti con i nuovi farmaci ad azione antivirale diretta di seconda generazione (DAAs) per la cura dell’epatite C cronica, raccolti dai Registri di monitoraggio AIFA.
Papilloma virus: 8 adulti su 10 infettati una volta nella vita, ma meno di metà giovani si vaccina
Circa l’80% delle persone sessualmente attive ha contratto, almeno una volta nella vita, l’infezione da HPV (Human Papilloma Virus). Ne sono stati individuati circa 200 ceppi, alcune dei quali sono…
Gestione farmacologica della malattia di Crohn da moderata a grave: linea guida
Gastroenterologia ed EpatologiaL’American Gastroenterological Association (AGA) ha pubblicato nuove linee guida cliniche per la gestione farmacologica...
Observations from ID and Beyond: Hot Takes from IDWeek: CDC, COVID, and Two Doses of Dalbavancin
Dr. Paul Sax shares a conversation held during IDWeek, in HIV and ID Observations.
Applicazione della nuova “Classification Guideline” relativa alle Variazioni all’AIC
La nuova Linea Guida sarà applicabile dal 15 gennaio 2026.
Integration of Tobacco-Cessation Interventions into Tuberculosis and HIV Care
New England Journal of Medicine, Ahead of Print.
Linee guida cliniche ACG: diagnosi e gestione delle condizioni premaligne gastriche
Gastroenterologia ed EpatologiaLe condizioni premalignanti gastriche (GPMC) sono comuni e includono la gastrite atrofica, la metaplasia intestinale gastrica, la displasia...
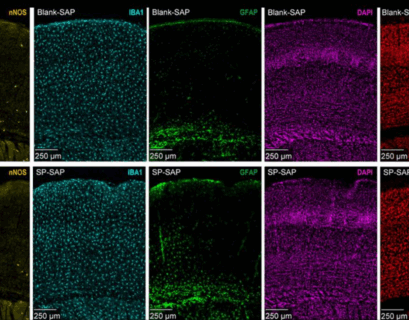
Lo stress può alterare il flusso sanguigno nel cervello
Notizie dalla RicercaI ricercatori della Pennsylvania State University hanno scoperto che un raro neurone sensibile allo stress, chiamato neurone nNOS di...
NICE: linee guida sul monitoraggio fetale durante il travaglio
Salute della DonnaQuesta linea guida in aggiornamento pubblicata da NICE, illustra i metodi per monitorare il benessere del bambino durante il...